HIQA publishes 2015 Overview Report of unannounced infection prevention and control inspections in 32 Irish hospitals
Significant increase in number of hospitals requiring re-inspection due to poor hygiene and maintenance.
Irish hospitals and staff have shown commitment and progress in improving hand hygiene practices, but poor levels of overall environmental cleanliness are exposing patients to the risk of Healthcare Associated Infections according to a new report, published today by the Health Information and Quality Authority (HIQA).
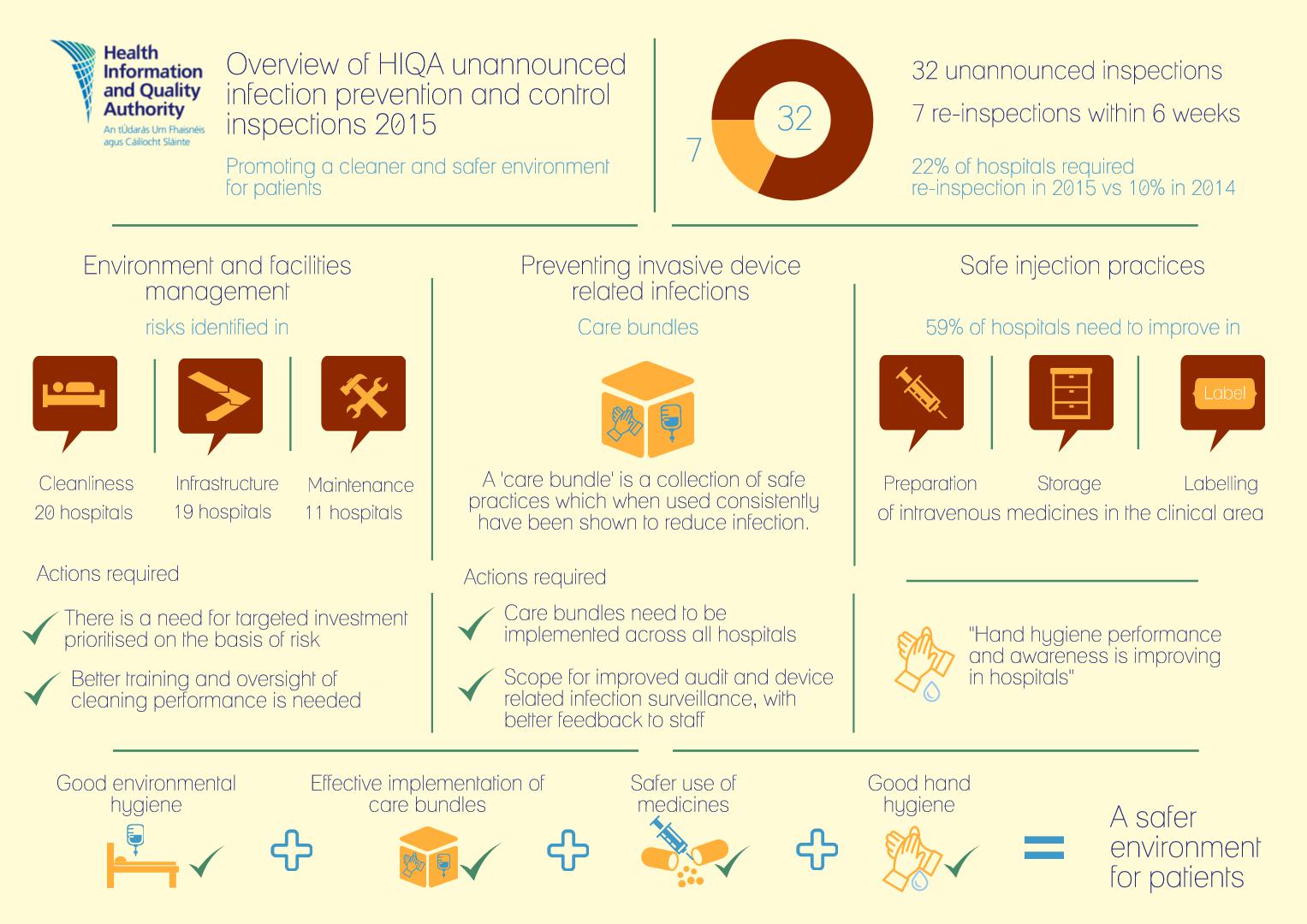
One in five hospitals inspected in 2015 required a follow-up inspection for poor hygiene and maintenance issues. This represents a significant increase compared to 2014 where one in ten hospitals required re-inspection.
Susan Cliffe, Head of Healthcare, HIQA said: “A clean and safe hospital environment is a fundamental expectation of patients, staff and visitors. An acceptable standard of basic cleanliness is both essential and achievable with better management and oversight of cleaning performance”.
Thirty-nine unannounced inspections were carried out by HIQA in 32 public acute hospitals between January 2015 and December 2015. The aim of these inspections was to assess compliance against the National Standards for the Prevention and Control of Healthcare Associated Infections. Seven of the 32 hospitals inspected required a follow-up inspection primarily due to poor hygiene standards observed during inspections and poor maintenance and management of the environment and facilities.
In six of the seven re-inspections, hospitals had addressed most of the risks indentified. However, no improvement in the standard of environmental hygiene was recorded in one hospital re-inspected. During the course of the 39 inspections, 64 clinical areas were inspected including high-risk areas such as operating theatres, endoscopy suites, haematology, oncology, intensive care and coronary care units.
Some re-occurring findings relating to infrastructural deficiencies and maintenance included units that were outdated with inadequate infrastructure from an infection prevention and control perspective. Overcrowding with limited spacing between beds was an issue for staff trying to circulate and manoeuvre patients. The lack of pro-active maintenance programmes resulted in worn and poorly maintained surfaces which do not facilitate effective cleaning.
The 2015 inspection programme saw the assessment of infection prevention care bundles for the first time. An infection prevention care bundle is a set of routinely applied evidence based actions that, when applied consistently, have been proven to reduce the incidence of infection and protect patients – this is particularly relevant in preventing infection through the use of invasive medical devices. While some hospitals have made significant progress in embedding the use of infection prevention care bundles into everyday practice, implementation is not as advanced in other hospitals. In these hospitals, policies, training and patient information must be improved to ensure compliance.
More than half of hospitals inspected in 2015 (59%) need to take action to improve the preparation, labelling and storage of intravenous medication in the clinical area. Failure to adhere to these practices potentially increases the risk of transmission of infection. Observations during inspections included pre-prepared syringes of medicines which were unlabelled or insufficiently labelled, inappropriately stored and left unattended and unsecured.
Susan Cliffe, Head of Healthcare, HIQA added: “It was evident during inspections in 2015 that overall, a greater culture of compliance with hand hygiene has begun to emerge in most hospitals. This observation is supported by the reported findings from the HSE national audits that have shown steady improvement over time.
“Infection prevention care bundles are also an important element of infection prevention and while effective implementation was identified in some hospitals, care bundles need to be implemented in all acute hospitals where they are not already in place. Good practice includes the reliable application of care bundle steps, accompanied by audit and feedback to staff on compliance with care bundle measures, and device related infection surveillance”.
During 2016, HIQA will continue its monitoring programme of unannounced inspections of public acute Irish hospitals to monitor compliance with the Infection Prevention and Control Standards. The focus of the inspections will build upon the approach and findings of 2015 with continued emphasis on areas that pose the highest risks to patients.
Ends.
Marty Whelan, Head of Communications and Stakeholder Engagement, HIQA
01 814 7480 / 086 2447 623 mwhelan@hiqa.ie
- HIQA’s unannounced inspections aim to assess the compliance of public acute hospitals against the National Standards for the Prevention and Control of Healthcare Associated Infections while continually promoting a reduction in Healthcare Associated Infections (HCAIs). Hospitals are assessed against three selected National Standards during an unannounced inspection - Standards 3, 6 and 8 of the Infection Prevention and Control Standards. These Standards focus on good hand hygiene compliance, well maintained hospitals with high standards of cleanliness and the implementation of care bundles, but other Standards may be observed and reported on if concerns arise during the course of an inspection.
- Re-inspections were carried out in some hospitals within six weeks of the first inspection where immediate high risks were identified during the initial inspection. The aim of the re-inspections was to promote rapid improvement in relation to the immediate high risks identified. Reports detailing the findings from the inspections are published on HIQA’s website. HIQA asks each hospital to publish a quality improvement plan within six weeks of the publication of an inspection report. The inspection team monitors the publication of the quality improvement plan and will review progress with implementing the plan during subsequent inspections.
- Re-inspections were carried out in the following hospitals:
- Kerry General Hospital, Tralee, Co. Kerry
- Letterkenny General Hospital, Co. Donegal
- Midland Regional Hospital at Mullingar, Co. Westmeath
- National Maternity Hospital, Holles Street, Dublin
- Our Lady of Lourdes Hospital, Drogheda, Co. Louth
- Portiuncula Hospital, Ballinasloe, Co. Galway
- South Infirmary Victoria University Hospital, Cork
- Care bundles are a group of evidence-based practices which, when applied together, can reduce the incidence of infection and protect patients. During the unannounced inspections, particular focus was placed on the implementation of peripheral and urinary catheter care bundles and the monitoring of device-related infections. While progress has been made in some hospitals with implementation, this has not been widespread. Those hospitals demonstrating a high level of compliance with Standard 8 had infection prevention care bundles embedded in practice across all areas of the hospital inspected with high staff awareness levels.